Diabetic Eye Disease: What You Need To Know
What is diabetes?
Diabetes is a common, chronic condition that occurs when your body is unable to regulate the amount of sugar in their blood, leading to various complications. There are two types of diabetes: Type 1 and Type 2. Type 1 diabetes typically affects younger individuals, has a rapid onset, and requires regular injections of insulin as their body is unable to produce it on its own. Type 2 diabetes is more gradual in its onset, affects older individuals, and is more easily managed by diet and exercise. Diabetes is estimated to impact about 10% of all Americans.
What is diabetic eye disease?
Diabetic eye disease refers to the group of ocular complications that can result from unmanaged diabetes. They include:
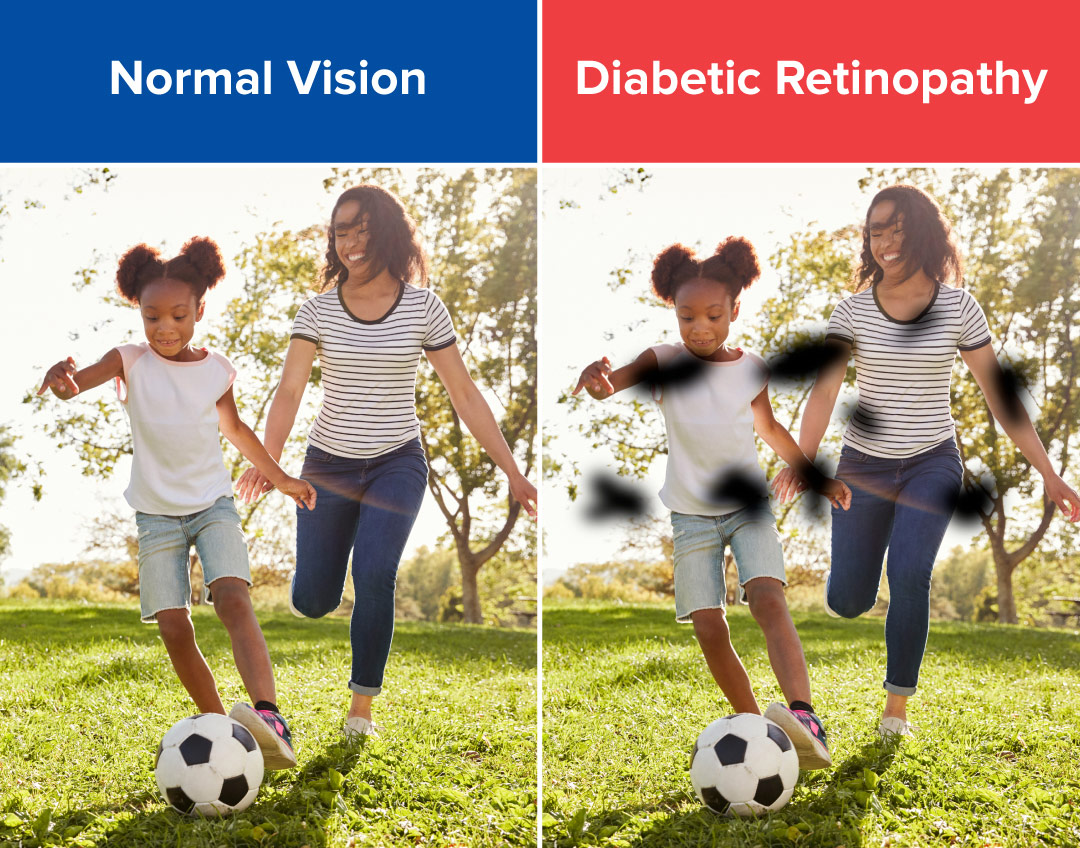
- Diabetic retinopathy: A condition that occurs when the blood vessels at the back of the eye (the retina) become damaged. While diabetic retinopathy may present with no symptoms initially, it can eventually lead to complete vision loss ifleft untreated. Symptoms include blurred vision, impaired color vision, or dark “empty” spots in vision. The longer you have unmanaged diabetes, the more likely you are to develop diabetic retinopathy.
Diabetic retinopathy is the most common cause of vision loss among those with diabetes and the leading cause of vision impairment and blindness among working-age adults. Between 40-45% of those diagnosed with diabetes already have some degree of diabetic retinopathy.
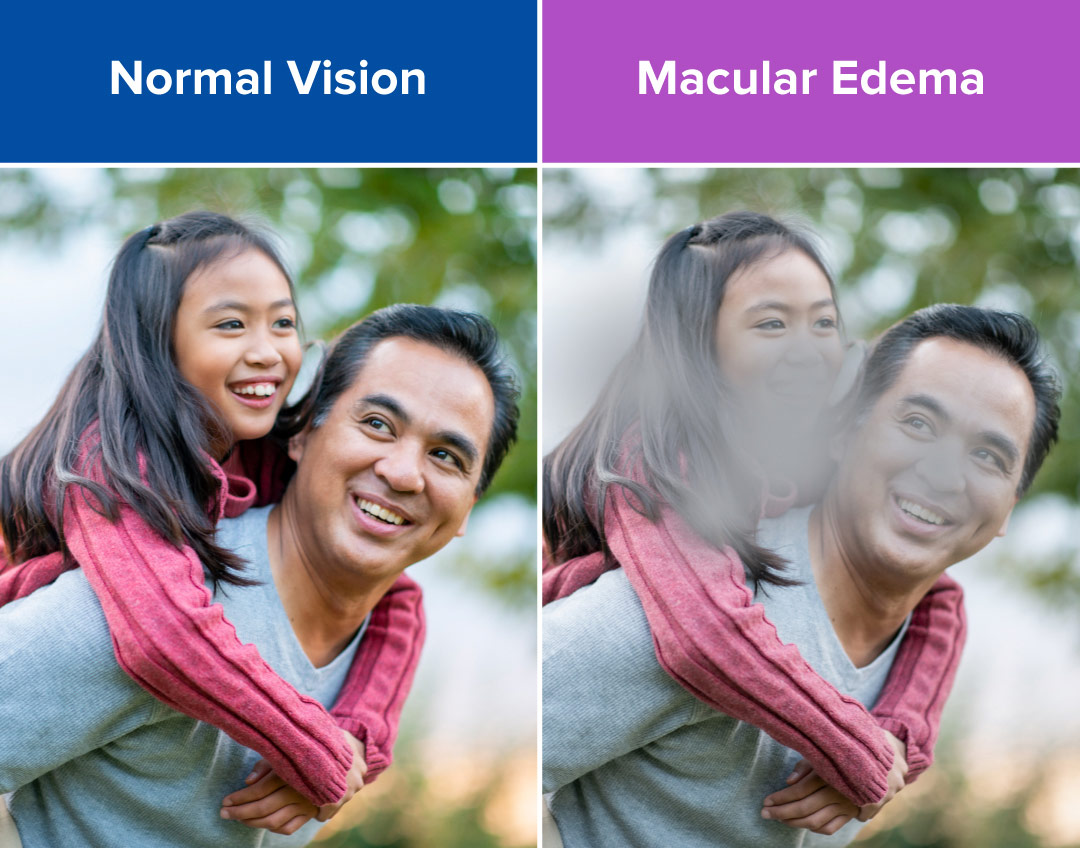
- Diabetic macular edema (DME): A condition in which fluid builds up in the macula (center of the retina). The primary symptom of diabetic macular edema is blurry or wavy vision in the center of your field of vision, which is needed for tasks that require detail such as reading or driving. It can also lead to a distortion or fading of color. Macular edemas often form as a result of diabetic retinopathy. Vision loss from DME can progress over a period of months and over time make it impossible to focus clearly. It affects about 10% of those with diabetes and will develop in about 50% of those with diabetic retinopathy.
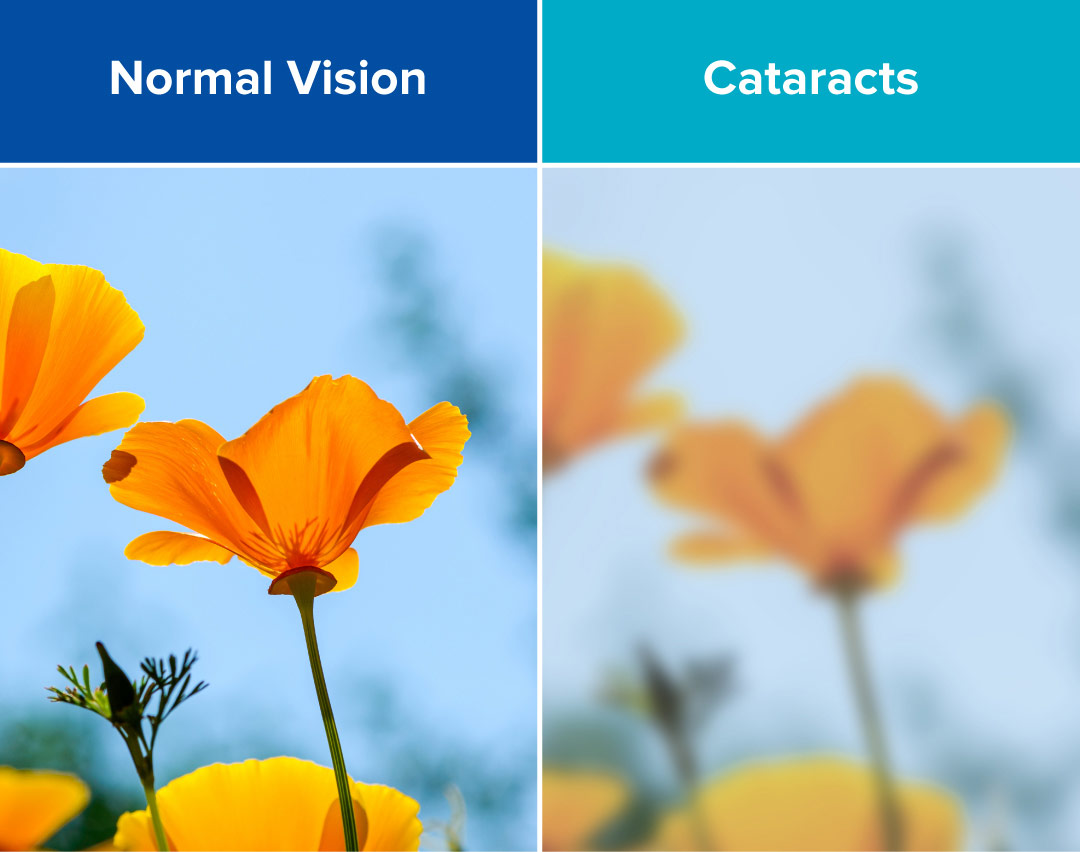
Cataracts: A condition involving the progressive clouding of the lens of the eye, obscuring vision the way that one would experience if they were looking through a foggy window. While cataracts are correlated with a number of factors, such as eye trauma or old age, diabetes is one of the key risk factors in developing cataracts and can increase your chances by as much as 60%.
As with most diabetic complications, managing your blood sugar is the best way to minimize the risk of their development.
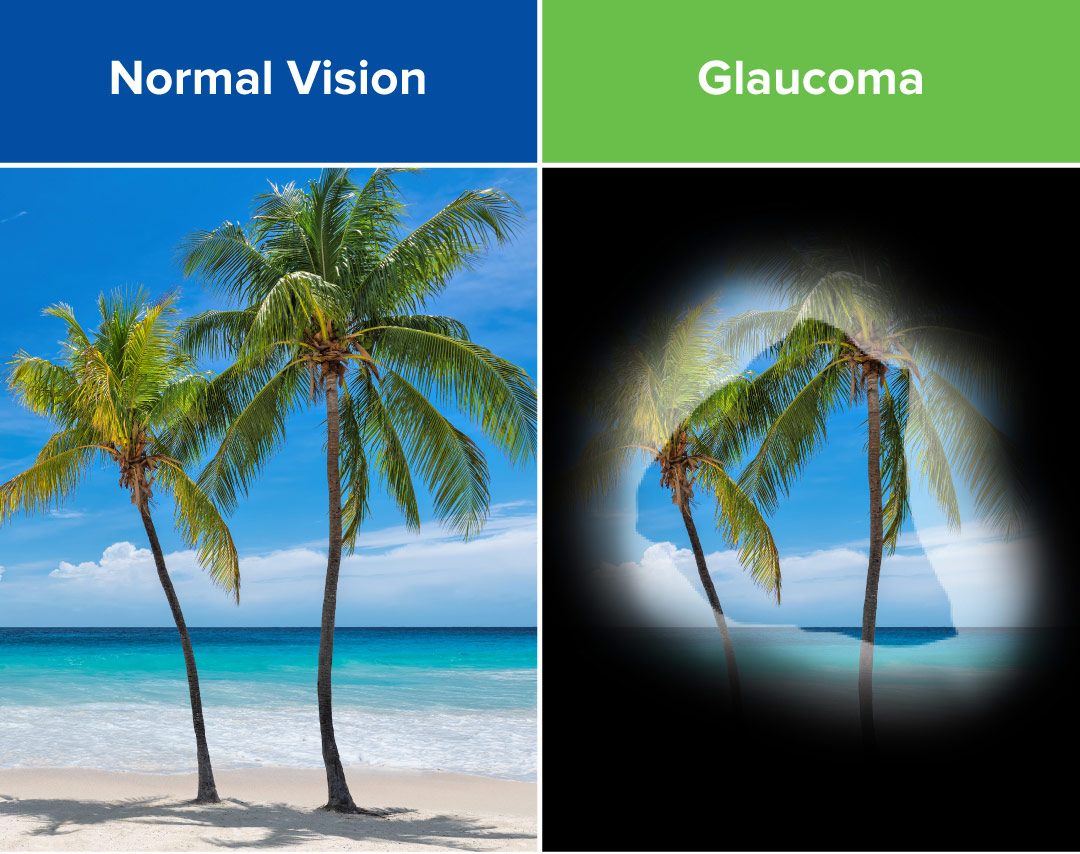
Glaucoma: A condition that occurs when there’s a buildup of ocular pressure in the eye, putting pressure on the optic nerve. Like a macular edema, glaucoma can be a byproduct of diabetic retinopathy. Referred to as the “silent thief of sight” because it has no symptoms in its earliest stages, 50% of those with glaucoma have no idea they have it. Glaucoma can result in a complete loss of vision if left untreated, and any vision lost is typically unrecoverable.
When should I see an eye doctor?
If you are diabetic, prediabetic, or at an increased risk for diabetes, it’s best to see an eye doctor once a year for a dilated eye exam - even if you’re not experiencing any vision problems. Your eye doctor will be able to detect early signs of any eye disease before symptoms begin to appear. Combined with blood sugar maintenance, working closely with your eye doctor is the best way to prevent vision loss from diabetes.